In a recent healthcare fraud case, from a short timeframe of November 2022 through May 2024, over $1.2 billion dollars in false and fraudulent claims was submitted to health insurance plans related to skin grafts. The fraudsters were paid more than $1 million dollars per patient for the unnecessary grafts and received $600 million from Medicare in 16 months alone1.
The high reimbursement amount for skin grafts makes them an attractive area for fraudsters to target. Looking at the Medicare ASP January 2025 Fee Schedule2 reimbursement amounts for some of the HCPCS codes associated with these products and the reimbursement fees can be as high as several thousands of dollars per a billable unit of 1 square centimeter. The reimbursement amount can quickly balloon per patient, especially with dollar amounts like that.
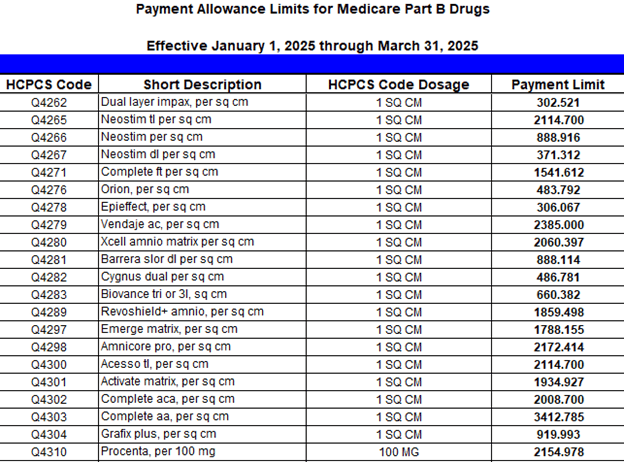
Figure 1. Medicare ASP January 2025 Fee Schedule
Per the Current Procedural Terminology (CPT) codebook definition3, skin substitute grafts include non-autologous human skin (dermal or epidermal, cellular and acellular) grafts, non-human skin substitute grafts, and biological products that form a sheet scaffolding for skin growth. The supply of skin grafts should be reported separately in conjunction with the application CPT codes further increasing reimbursement. The ambiguity or even the absence of medical necessity policies makes the reimbursement of skin grafts rife for fraud.
To avoid inappropriate payments for costly skin grafts, Context4 Healthcare (C4H) recommends that your Plan creates a skin graft policy. Several Medicare Administrative Contractors (MACs) publish related Local Coverage Policies that can be used as a reference. Your policy should list CPT and HCPCS codes along with the supportive diagnosis codes. Require detailed documentation of wound size and description, other standard of care interventions attempted, progress of healing, reasons for use of the skin substitute graft, and a case specific plan with reasonable expectations. And finally, audit supportive medical records frequently.
In auditing these records, be familiar with the standards of care for the type of wound treated. Require a detailed op-note relevant to each date of service you audit. Be familiar with the type of skin substitute used in the case, and confirm it matches appropriately with that clinical scenario. Expect the wound care plan to be documented in the report, and well as some statement about the progress of healing. As you audit, watch out for cloned, generic, or ambiguous documentation. For each encounter audited, require that your providers document each skin substitute used was a medically necessary aspect of that beneficiary’s wound care plan.
Your fraud waste and abuse reports must help you efficiently monitor frequency of skin substitute graft procedures and isolate pertinent claims for auditing. C4H offers several FWA reports, one that identifies the most frequent codes billed related to skin grafts and another that identifies the highest billed amounts per provider. To find out more, visit C4H Payment Integrity webpage for more information: https://www.context4healthcare.com/solutions/medical-payment-integrity/
References:
- https://www.justice.gov/opa/pr/arizona-couple-pleads-guilty-12b-health-care-fraud
- https://www.cms.gov/medicare/payment/part-b-drugs/asp-pricing-files
- AMA 2025 Current Procedural Terminology

